It may seem strange, but I don’t remember the day that I actually learned that my mother has a chronic, life-altering disease. She says that she and my father sat me down as a child and explained that she has Multiple Sclerosis (MS). As hard as I try, I can’t remember any memories of that discussion from the mix of micro-memories I still have of my younger years. You may be asking, “What is MS, exactly?” Funnily enough, even though it affects my family’s day-to-day life in very real ways, I didn’t fully understand what it was until very recently. While taking a Medical Decision-Making class last semester, I had the opportunity to do a research project to close out the semester. Naturally, I thought this would be the perfect opportunity to learn more about MS while also raising awareness around this autoimmune condition.
MS is a chronic disease that attacks the central nervous system (CNS). A normal nerve fiber (axon) is wrapped in multiple layers of myelin, a protective coating which allows electrical signals to travel quickly and efficiently. In patients with MS, the immune system attacks and damages the myelin sheath in the brain and spinal cord. Areas of myelin become inflamed and damaged, leaving exposed segments of axon that conduct signals poorly or not at all. This disrupts communication between the brain and the body. Although MS presents differently in each patient, it often causes problems with movement, sensation, vision, speech, and other bodily functions.
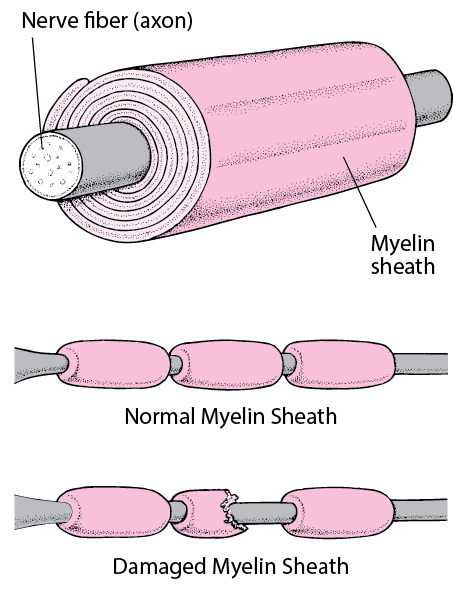
As MS progresses, the repeated injury to myelin and underlying axons can lead to permanent scarring and loss of nerve fibers. As the MS Society explains on their website, this permanent damage can cause long-term disability, including physical and cognitive decline, extreme fatigue, muscle weakness, spasms, severe balance issues, vision loss, bladder/bowel dysfunction, chronic pain, and significant cognitive issues such as memory loss and difficulty thinking clearly. The condition can also lead to paralysis, difficulties swallowing, increased risk of infections, and emotional problems like depression and mood swings.
For my mother, fatigue is just one of the major MS symptoms that she struggles with. I suspect people may think, “I get tired too, and I don’t have MS.” The truth is, however, that MS fatigue is not your typical fatigue; it’s a whole different beast. When I was little, my mom would use a spoon analogy to explain her energy in comparison to other individuals without an autoimmune condition. In this analogy, “spoons” represent our energy to function like a normal human being. When you’re out of “spoons,” you have absolutely nothing left to give. With no spoons, you can no longer manage even normal, daily tasks. As my mom explains, “Let’s say that most people start their day with 100 spoons. If that’s the case, I would say that I start my day with a quarter of that, at best.” She starts with a very low number of spoons, and everything she does costs her some of those few, precious spoons. As she explained, “It’s not just the normal stuff that you’d expect to zap your energy, like working out or accomplishing some huge task. I mean literally everything: showering, walking the kids to the bus, cooking a meal, doing laundry, meeting with a teacher, or even something leisurely like meeting a friend for coffee. It all costs me spoons, and it generally costs way more spoons than you’d expect. Over the course of the past 18 years, the number of spoons I start with on any given day has dwindled drastically.” After her latest massive flare in 2021, she has experienced a significant decline. This change has not come through by obvious flares, but rather it has manifested as “silent but undeniable deterioration.” My mother stated that living with MS means she has “to be shamelessly selective” in prioritizing what she gives her energy to in order to avoid being in a “spoon deficit.”
Once I understood what MS was, I became curious about how different healthcare systems shape the experience of those suffering from the disease. Having a mother who lived in both the US and France, I had heard stories about the experience of treatment and care in both nations. Ultimately, I decided to focus my research on the comparison of the French and the US MS treatment and care. To begin, I interviewed my mother to learn about how the French and American healthcare systems had affected her.
First, I focused on France, which has a universal coverage system and classifies MS as “affection longue durée.” This status provides 100% coverage for treatment, doctor visits, tests, MRIs, and medication, allowing patients to focus on their health instead of worrying about financial costs. While France has both public and private hospitals, my mother’s experience was entirely within the public system, where MS care is standardized and fully funded. When it comes to actual treatment options, France has a more conservative approach towards new therapies as they require thorough safety data before approval.
In contrast, the US has an insurance-based system. This means that the patients’ access is directly tied to whether they have private insurance. When my mother was diagnosed in France after recently moving there straight out of college, her neurologist in the US warned her not to cancel her US insurance due to the very real risk of being denied later. This highlights how the US system makes it difficult for patients to get insurance if they have a pre-existing condition. I also learned in the interview that treatment and medications are very expensive, casting a high financial burden and often causing anxiety for the patient. It is worth noting that discount programs do exist to help patients pay for their treatments, but they are often difficult to navigate, further adding stress onto MS patients. A final interesting fact that I learned is that the US is often faster at adopting new therapies, and neurologists are able to prescribe aggressive treatments without a long approval process.
After the interview, I wanted to explore these differences further and began researching online.
In France, as I previously mentioned, this condition is classified as “affection longue durée” (long-term disease), ensuring coverage for most patients, making it easier to access to neurologists and medications, and also having lower direct costs for patients. During my research, I discovered that the mean cost per MS patient is around $27,000 per year. This is not what patients personally pay, but rather what the government pays in terms of certain factors, including drugs, consultations, equipment, and more. The cost per QALY (quality-adjusted life year) in France is around $40,000 to $60,000 (this system is used to figure out the cost-effectiveness of treatments and how much it costs for a better life or survival in another year.) However, despite universal coverage, MS patients still face out-of-pocket expenses (OOPE). A study showed that over 60% of patients in one study struggled to choose between MS-related expenses and family/social spending. Some examples of OOPEs are non-prescription meds, home adaptations, home care services, and more.
In the US, as I mentioned earlier, insurance determines access to treatment and care, leading to major differences in cost and patient experience. Research revealed that the mean cost per MS patient was greater than $60,000 per year, significantly higher than France. In the US, the disease modifying treatment (DMT) pricing is also greatly larger. US MS drugs are two to three times more expensive than in France, further demonstrating the difference in healthcare costs. In addition to this, the cost per QALY is around $900,000 per year (compared to the French cost per QALY of $40,000 – 60,000). Despite this massive cost gap, US based care demonstrates only modest gains in health and lifespan for the patient.
Overall, there’s a noticeable difference between the American and the French healthcare systems. France offers stability and affordability, but appears to be slightly less aggressive in adapting new treatments. The US system, on the other hand, tends to adopt new therapies more quickly, but leaves patients dealing with far higher cost and uncertainty.
This project was extremely informative to me on a personal level, but it also opened my eyes to the important issue of healthcare inequality. Rising drug prices and access barriers affect many chronic conditions, not just MS patients. When healthcare costs are high, patients are more likely to skip or delay treatment. If healthcare costs continue to soar, health outcomes will worsen, and families will increasingly be forced to choose between healthcare and basic living expenses. By understanding these differences, we can work to push us for a fairer, more sustainable healthcare system.
If you’re interested in learning more about this topic, you can do something as simple as following someone with a chronic condition or disability on social media to learn more about how the diagnosis and healthcare system impacts their life. If you would like to make an even greater impact, I encourage you to donate to France Sclérose en Plaques or to National Multiple Sclerosis Society in the US.
Works Cited
Hartung, Daniel M, et al. “The Cost of Multiple Sclerosis Drugs in the US and the Pharmaceutical Industry: Too Big to Fail?” Neurology, U.S. National Library of Medicine, 26 May 2015, pmc.ncbi.nlm.nih.gov/articles/PMC4451044/.
Heinzlef, Olivier, et al. “Economic Burden of the Out-of-Pocket Expenses for People with Multiple Sclerosis in France.” PharmacoEconomics – Open, U.S. National Library of Medicine, Dec. 2020, pmc.ncbi.nlm.nih.gov/articles/PMC7688762/.
Kanavos, Panos, et al. The IMPrESS (International Multiple Sclerosis Study): Socio-Economic Burden, Health Related Quality of Life and Experiences of Multiple Sclerosis Patients in France. London School of Economics and Political Science, 2016, eprints.lse.ac.uk/68478/1/Results_of_the_socio-economic_burden_author.pdf.
Mikulic, Matej. “Multiple Sclerosis Drug Prices International Comparison to US 2018.” Statista, 20 July 2020, www.statista.com/statistics/1134367/ms-drug-prices-international-average-vs-us/.
“Multiple Sclerosis.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 1 Nov. 2024, www.mayoclinic.org/diseases-conditions/multiple-sclerosis/symptoms-causes/syc-20350269.
Noyes, K, et al. “Cost-Effectiveness of Disease-Modifying Therapy for Multiple Sclerosis: A Population-Based Study.” Neurology, U.S. National Library of Medicine, 26 July 2011, pmc.ncbi.nlm.nih.gov/articles/PMC3140799/.
Simoens, Steven. “Societal Economic Burden of Multiple Sclerosis and Cost-Effectiveness of Disease-Modifying Therapies.” Frontiers, Frontiers, 2 Dec. 2025, www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2022.1015256/full.
“What Is Advanced MS?” Ms Society, www.mssociety.org.uk/living-with-ms/advanced-ms.